health psychology Notes
Module 5.1: Determinants of Health
What will you learn in this section?
- Models of health
- The biomedical model concentrates on biological causes and treatments for illnesses
- The biopsychosocial model is far more complex and takes into account biological, psychological, and social causes and treatments for illness
- Determinants of health
- Social and personal determinants of health
- Risk and protective factors: many factors affect our health, some in positive ways
- How health beliefs can affect the health of the individual.
Biomedical model
- The biomedical model represents an attempt to understand disease (and human behavior) as a result of biological processes in the body.
- It leaves no room in the framework for social or cognitive influences (for example, the built environment, socio- economic status, appraisals and decision making) on health or wellness. The main assumption made by the model is that illnesses can be attributed to somatic (physical) causes such as biochemical imbalances or neurological abnormalities.
- Hidden in this assumption is the belief that your brain is the only determinant of your psychology and your mental self; essentially the mind exists only as a result of the brain.
- It is therefore a reductionist model as it explains complex phenomena from a simple biological approach. Carl Sagan (1977) arguably supports this model with his claim that, “my fundamental premise about the brain is that its workings—what we sometimes call ‘mind’—are a consequence of its anatomy and physiology, and nothing more”
- The use of the biomedical model had a tremendous impact on how illness was perceived and treated until the 1970s.
- In the twentieth century, this model was moderated by the introduction of psychosomatic
and behavioral medicine. Psychosomatic as a word is a combination of psych {mind} and soma(body). So there was an acknowledgement of the role of mind in health. and the introduction of behavioral medicine introduced the idea of preventative medicine changing how an individual behaves to maintain health. - Health psychology as a discipline sees illness differently from the biomedical model. It does not regard poor health as having a purely biological cause and has replaced this idea with the health of an individual being due to a complex system of interacting forces. This is a holistic viewpoint.
- The shift means that they see an individual is responsible for their own health.
- Treatment is advocated using a series of professionals who can help with all aspects;no longer seen as the domain of doctors only
- Health is ultimately seen as an interaction between body and mind. One model which acknowledges this interaction is the biopsychosocial model.
Biopsychosocial model
This model acknowledges both the influence of biology and psychology in illness but also highlights the influence of environmental factors such as poverty and working conditions. It was developed by Engel and is an integrative model.
Engel stated that there were three key elements to health and illness:
a. Biology
b. Psychology
c. Social
All the above have relatively equal influence on health.
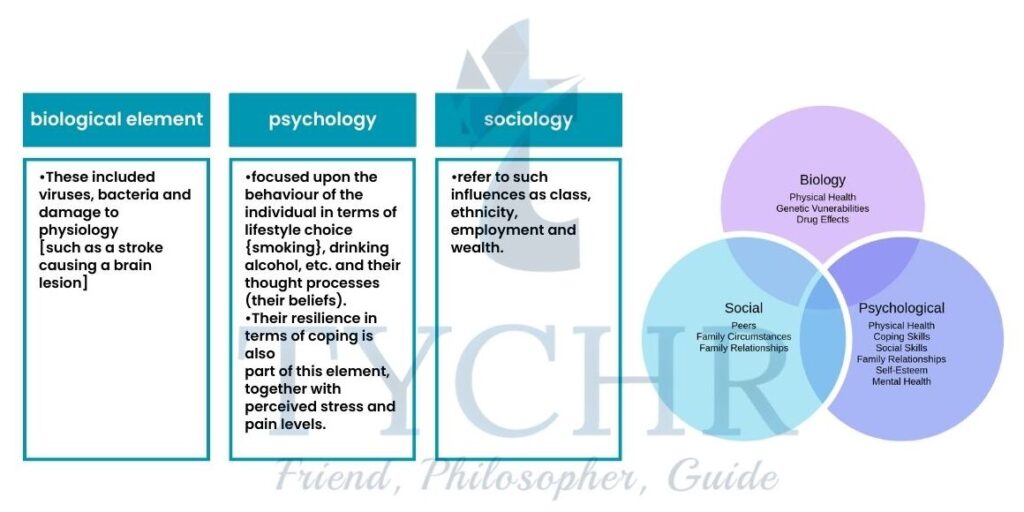
NOTE :-
Culture too plays a part in the model at this level. A culture can determine whether an individual is likely to seek help for their medical problem, or not. It can equally affect the adoption of protective behaviors to maintain good health.
An example of this is screening or illness or inoculation against illness. Subcultures too can have an effect.
For example, Zola [1966) noticed that Italian Americans report a larger number of symptoms than Irish Americans. However, the Irish Americans reported many more issues with respiratory problems, particularly the ear, nose and throat. There is no clear reason for this difference other than cultural norms.
- The BPS model comparative to the biomedical model is less oversimplified and hence and therefore accounts for more number of variables which allows for more holistic study of behavior.
- Its thoroughness could imply that all the three analysis levels are always of interest during the determination of illness but it is not considered at each level of the relative contributions. In fact, it is possible that some behaviors or health problems can be treated successfully with just one or two elements from of this model
Determinants of health

The range of social, economic, environmental and personal factors that influence health and wellbeing are known as the determinants of health. These measures are used by governments and policy-makers to design interventions in areas where health inequalities are negatively impacting the health and wellness of a group of people. The determinants of health can be broken into two main categories:
a)social determinants of health :- includes all other determinants of health such as the social and physical environment and access to health care.
b)personal determinants of health :- includes individual behavior and geneticsResearchers for the most part perceive five determinants of strength of a populace, which are:
- social environment
- physical environment
- health services
- biology/genetics
- individual behavior.
Health risks and protective factors
- Health-care professionals typically organize factors related to wellness and illness into two categories: risk factors or protective factors
- A risk factor is any attribute, characteristic or vulnerability of an individual that increases the chances of growing a condition, disease or injury. For example, exposure to cheap, easily accessible junk food and a permissive environment may increase the likelihood of an individual becoming obese; this in turn will increase an individual’s chances of developing type 2 diabetes, cardiovascular disease and other illnesses.
- Some examples of the more important risk factors include obesity, being underweight, unsafe sex, high blood pressure, tobacco and alcohol consumption, and unsafe water, sanitation and hygiene. Protective factors include regular exercise, a healthy diet and access to clean water.
Module 5.2: Health problem 1: obesity
What will you learn in this section?
Health problem—obesity
- Obesity risk factors (inactivity, poor diet, genetics, family environment, socio-economic status) and protective factors (physical exercise, healthy eating)
- Social determinants:
poverty contributes to obesity (Beheshti, Igusa and Jones-Smith, 2016) - Biological determinants:
sugar is argued to be the main culprit for the current obesity epidemic (Lustig, 2015) - Cognitive determinants:
being overly optimistic can set up obese dieters for failure; an internal locus of control
- Overweight and obesity have been defined as a state where an individual has accumulated excess body fat to the point that it affects health. The most commonly used metric for measuring overweight and obesity is the body mass index (BMI)
- BMI was devised in the 19th century by Lambert Adolphe Jacques Quetelet. It is expressed as body mass divided by the square of the body height. Many criticize the index as an inadequate measure of overweight and obesity.
BMI is calculated using the formula: Metric:
BMI = weight(kg)/height2(m2)
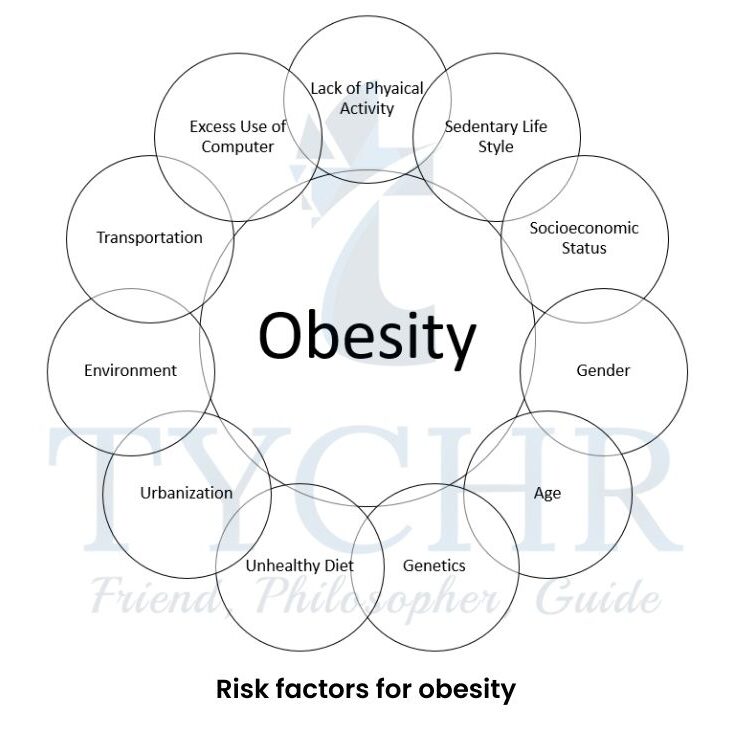
Risk factors for obesity
- Inactivity, leading a sedentary lifestyle, can increase your
chances of being obese. - Eating an unhealthy diet high in salt and sugar has been linked to obesity.
- Our genes may have an impact on how much fat we store in our bodies or how obesity affects our metabolism.
- Family environment—obesity tends to run in families; you develop eating and exercise patterns from your family.
Socio-economic status, poverty and obesity appear to be linked. More nutritious foods are more expensive and access to safe areas for exercise requires time and money.
Consequences of Obesity
- Type 2 diabetes: ang-term metabolic disease that is characterized by high blood sugar, insulin resistance, and relative lack of insulin.
- Hypertension: abnormally high blood pressure.
- Some cancers: cancer of the breast (post-menopausal), uterus, pancreas, gallbladder, liver, esophagus, kidney, thyroid and ovaries. Risk is also increased for blood cell cancers, including myeloma, leukemia and non-Hodgkin lymphoma.
- Cardiovascular disease: a type of disease which is related to the heart or the arteries. It generally involves heart attack and angina
1. Social Determinants of Obesity
Two things that seem to play a role in the recent pandemic of obesity are a
1. sedentary lifestyle and
2. the type of foods we consume.

1. Sedentary life
Very simply, we store energy and become obese when the amount of energy consumed is greater than the amount of energy used by our
bodies. A sedentary lifestyle uses less energy than an active one. Sedentary behaviors include screen-time activities, commuting in a car,
eating or working on a computer.
WHO warned that physical inactivity was a leading cause of disability and disease (WHO, 2002).
2. Types of foods we eat
Discretionary calories are defined as the difference between total energy requirements and the energy consumed to meet recommended nutrient intakes. Discretionary calories are allowable only “when the amount of calories used to meet recommended nutrient intakes is less than the total daily calorie expenditure” (USDA).
So by eating nutrient-rich foods, you are getting the most caloric
“bang for your nutritional buck” and will more likely have
discretionary calories to “spend” as you like throughout the day.
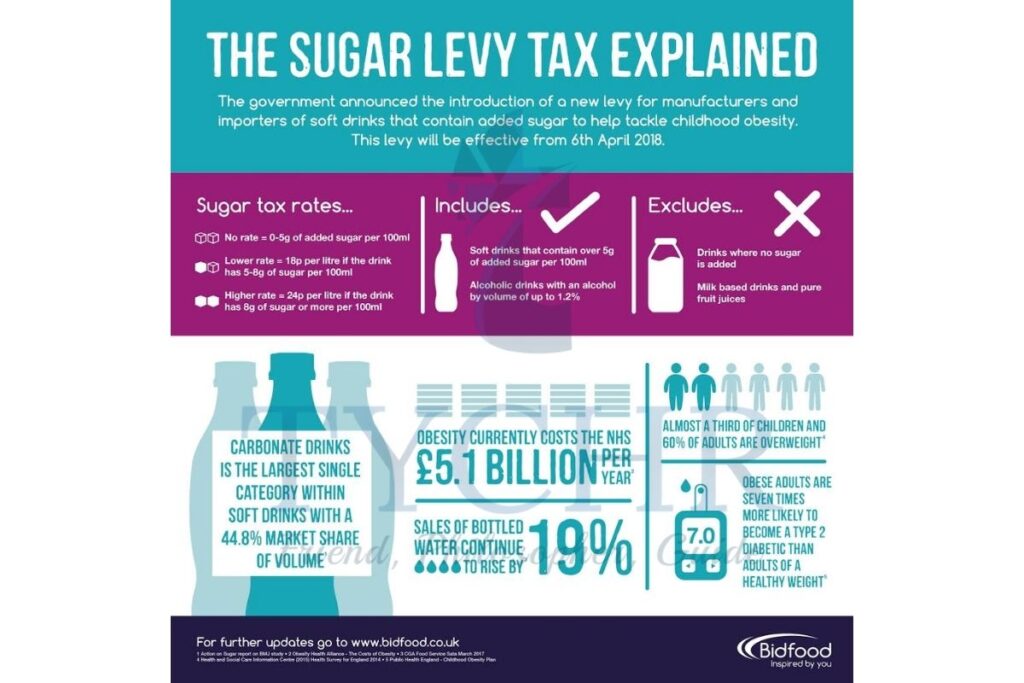
- Our food environment has changed dramatically in the past 40 years. One marker in particular stands out: soft drinks or sugar- sweetened beverages (SSBs). SSBs are the number one source of added sugars in Americans’ diets (Johnson et al, 2009). An increase in the consumption of SSBs has been linked to the increase in obesity in the USA. The Center for Science in the Public Interest has reported that in 2013 American adults consumed an average of 144.5 liters of SSBs. The following information is from their 2015 report entitled “Carbonating the World”.
- An extra 12-ounce sugary drink a day increases a child’s risk of becoming obese by about 60%.
- Adults who consume one sugar sweetened drink or more than one, they are 27% more likely to be overweight as compared to non drinkers Each year, approximately 180,000 people worldwide die from SSBs, including:.
- 133,000 to diabetes
o44,000 to cardiovascular disease
o6,000 to cancer
- Our food environment is rife with packaged and processed foods that have added sugars. This not only happens in sweets and candies but in nearly all processed foodstuffs such as pasta sauces, potato chips and ketchup.
- The term “added” is key because most foods already contain sugars that
are healthy and natural like those found in milk and fruits. For example, 250 milliliters of chocolate milk has over 10 grams more sugar than white milk. - Added sugars are often referred to as “empty calories”. They are empty because there is no nutritive value to the sugars; they are simply energy to be used or stored. The average American consumes 88 grams of sugar each day but the American Heart Association advises not to exceed the limit of30 grams each day (Harvard, 2017).
- Often those living in poverty have no choice but to buy calorie-dense foods, even if those calories are empty and do not contain any nutritional value. Empty calories are cheap calories. The fact that low-income families tend to buy nutrient-dense, high- sugar and fatty foods is reinforced by a 2016 article in the Journal of Nutrition which found that low-income consumers use a price/calorie model when deciding on food purchases.
2. BIOLOGICAL DETERMINANTS OF OBESITY
- Lustig agues that there are two biological mechanisms that are driving the obesity pandemic:
1.metabolism and
2.addiction. - In short, Lustig argues that fat in our diet is not the problem, sugar is. Lustig claims sugar is a chronic, dose-dependent hepatic (liver) toxin.
- The obesity metabolic syndrome is the name given to the relationship between obesity and its related diseases, including type 2 diabetes, hypertension, heart disease and lipid problems. Obesity is simply a marker for those diseases. The cause of the diseases is the biological process that underlies our metabolic processes.
- According to Lustig, it is biochemistry and hormones that guide our eating behavior.
- Leptin is a hormone that travels from your fat cells to your brain to tell it that you have had enough food and that energy burning can happen at a normal rate. However, for some reason and despite the higher levels of fat and therefore leptin, obese individuals have developed a leptin resistance where they no longer receive the message that their body has had enough food.

- This is where Lustig claims to be on the path to an answer. His claim is that the answer lies in the fact that insulin initiates a process to store sugar in fat cells in individuals who are already obese and live a sedentary lifestyle.
When we consume sugar, insulin levels rise to metabolize the incoming glucose and fructose. Work done by Lustig and his team shows that higher levels of insulin block leptin from reaching the receptors in the brain. The higher the insulin levels, the more energy you store and the hungrier you feel - Another argument for biochemical determination of eating behavior is addiction.
- Addiction is related to a reward pathway in our brain that releases the pleasure hormone dopamine in response to certain behaviors.
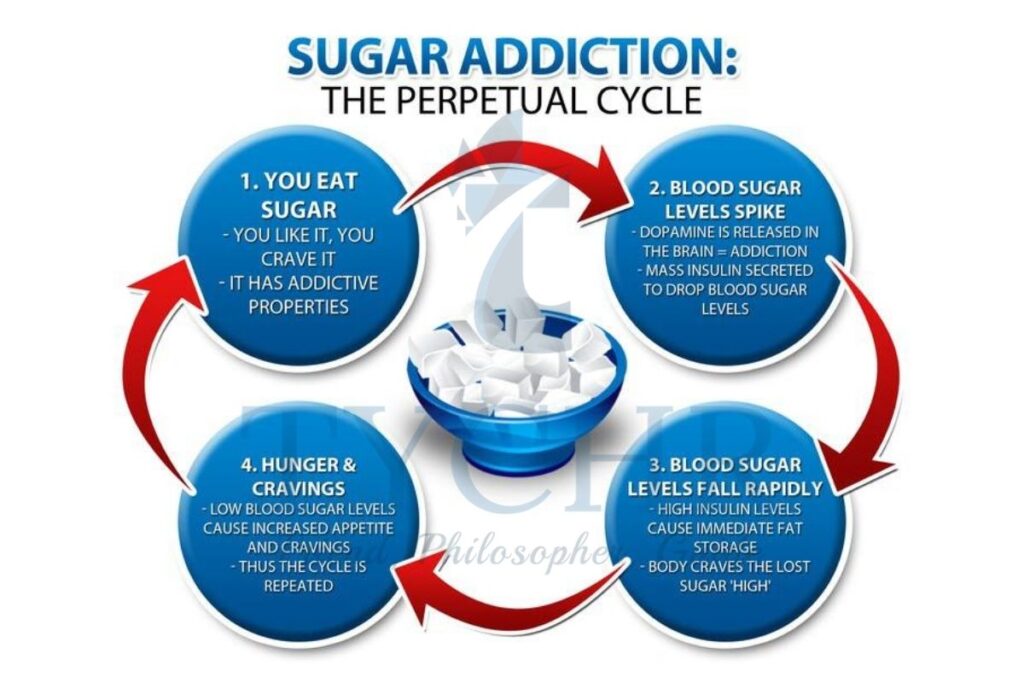
- This system is attached to certain parts of the brain which is responsible for controlling behavior and memory function. Food, and especially high-sugar and fatty food, causes the mesolimbic dopamine reward system (MDRS) to release dopamine in the nucleus. We are rewarded with a dopamine “hit” when we eat sugary or fatty foods that creates a feeling of pleasure.
- When we are constantly eating these foods and receiving the dopamine, it is possible to develop a tolerance for the dopamine, which will dampen its effect. In this case, after chronic stimulation of the MDRS, dopamine receptors begin to down regulate to accommodate for the higher levels of dopamine and tolerance is the result.
- To overcome the tolerance, more food is necessary to achieve the same dopamine effect. This leads to overconsumption of food Following on from the concept of tolerance comes withdrawal. If the source of the increased dopamine (sugary, fatty foods) is removed, then there is a drop in the amount of dopamine coupled with fewer receptors. This results in the individual experiencing withdrawal symptoms. In some ways, it seems that food addiction among obese individuals can be similar to psychoactive drug dependence (Lustig, 2014). This is by no means a universally agreed-upon fact but evidence is growing that food may act on the MDRS in a similar way to a psychoactive drug
The next big biological determinant that influences obesity is genetics. Our behavior is more complex than simple genetic programming (although not even that is simple). Family members are likely to share many of the same genes. If certain genes are responsible for obesity, then it can be expected that families would share obese characteristics. One problem with this, as Robert Sapolsky (2009) points out is that, “not only do genes run in families, environments do
too”. Due to the close social and environmental experiences of family members, reasons for obesity are difficult to assign to genetics or environmental similarities. This is known as the contamination effect.
- One last point on biological determinism comes from prenatal exposure to poor diets.
- Research on rats has shown that rat fetuses in the uterus of a mother with diabetes, overnutrition or obesity have a higher risk of becoming obese in their lifetimes. (Catalano and Ehrenberg, 2006).
- Additional research on rats has shown that exposure to a junk food diet in uterus and while breastfeeding is associated with an increased preference for and intake of fat in early life
- This suggests that the offspring of a snack-food eating mother will have a predisposition to fattier foods and a heightened dopamine-related response in early life (Ong and Muhlhausler, 2011)
3.COGNITIVE APPROACH TO OBESITY
- One of the main pillars of Lustig’s research is based upon the cognitive restraint theory.
- When we are hungry, a hormone called ghrelin is released from the gastrointestinal tract and binds to receptors on the hypothalamus. Ghrelin essentially has the opposite effect of the hormone leptin; its message to the hypothalamus is: “you’re hungry, consume something”.
- People who are attempting to eat less are essentially trying to ignore these messages with cognitive restraint (similar to willpower). In other words, they are trying to tell themselves they are not hungry when their biological system is telling them they are.
- This sort of cognitive-biological in getting must be
resolved, but the trouble is that you can’t make yourself
feel full just by thinking it. - If your hypothalamus is binding with ghrelin you will experience a biological drive to eat. This cannot be
ignored or “restrained” by willpower for an extended
period of time. - However, the types of food we eat are important and we can overcome the odds of becoming obese by simply adjusting our diets.
- Foods with high nutritive value and relatively low calories can stop ghrelin and initiate the release of leptin, signaling that we are full. So perhaps instead of limiting the amount of food we eat, it would be best to limit the food we eat to certain healthy foods which are high in nutrient value and low in added sugar.
- Sharot (2011) points out that optimism bias is a common
cognitive bias where we are less likely to believe that negative outcomes will happen to us. This false optimism could translate into many negative behaviors including overeating and “cheating” on a diet, as we exhibit a cognitive bias against unwanted outcomes and towards positive outcomes. For example, you might think, “I can have this soft drink and it won’t affect my diet. After all, it’s only one soft drink”. - When repeated attempts at losing weight fail, obese dieters may develop learned helplessness. In 1972,
- Martin Seligman proposed that when an organism perceives a loss of control in a situation and faces repeated failures, that organism may abandon any future attempt to achieve related goals. In other words, organisms learn that they are helpless and give up.
- Seligman contextualized learned helplessness as a precursor to depression. In the case of dieting and obesity, it may explain why some obese people come to accept obesity, and the eventual related diseases, as unavoidable facts of life (and death).
- Learned helplessness, in turn, is related to the concept of locus of control.
- Locus of control refers to the belief in the location (either internal or external) of an individual’s control over a situation or behavior. If individuals perceive the locus of control to be internal, they will have a stronger belief that they can change their behavior for the better.
- Locus of control is very closely related to Bandura’s concept of self efficacy. A belief in an internal locus of control results in strong self-efficacy.
- Success in meeting goals reinforces self-efficacy while failures erode it. A strong self-efficacy can result in persistence and perseverance in both improved food choices and exercise. Both of these have been shown to be protective factors against obesity.
Module 5.3: Social cognitive explanations of health problems
What will you learn in this section?
- Models of health behaviour— decision-making and health choices
- Theory of planned behaviour (Ajzen, 1985); application of the theory of planned behaviour to health (Conner and Sparks, 2005)
- Health belief model (Hochbaum, Rosenstock and Kegels)
- The theory of planned behavior, the health belief model and protection motivation theory are essentially models of decision-making.
- Each of these models represents an attempt to explain the thought process that occurs between an observable stimulus and a related behavior (Abraham, 2008). In other words, these models try to explain what happens in an individual’s mind when they are trying to decide how to act in a given situation. Why does a person smoke, drink alcohol or engage in risky sexual behavior?]
- Models of health behavior attempt to predict and change negative health behavior and decisions by first understanding how those decisions are made.
Health Belief Model
- This model was generated in the 1970 to understand why preventative behaviors were not employed by individuals to protect their health. The take-up rate of screening, for example, was lower than expected.
- It provides a way to ascertain the likelihood of someone using the facilities and services available to them, adding insight into the actions of the population.
- Likelihood of engagement is established by looking at how at risk individuals feel they are and whether they evaluate the service facility positively.
- There are key elements in the model centered on
- individual perceptions,
- modifying factors
- and likelihood of acting.
Individual Perceptions | Modifying Factors | Likelihood of acting |
| Perceived threat is a combination of both perceived susceptibility and perceived severity. In other words, “how likely is it that I will get it?”and “if I get it, how bad will it be?” The assumption here is that if an individual perceives that he or she is likely to get sick with a serious illness, then that person is likely to act in a way that will prevent the outcome.the perceived susceptibility to the consequences of not acting and the perceived severity of not acting (It will kill me, or am I at risk with the intervention?) influence the behavior | Modifying factors include the
| The likelihood of action relates to the costs, barriers and benefits of acting, for example the accessibility of a service or the likelihoodof making friends. |
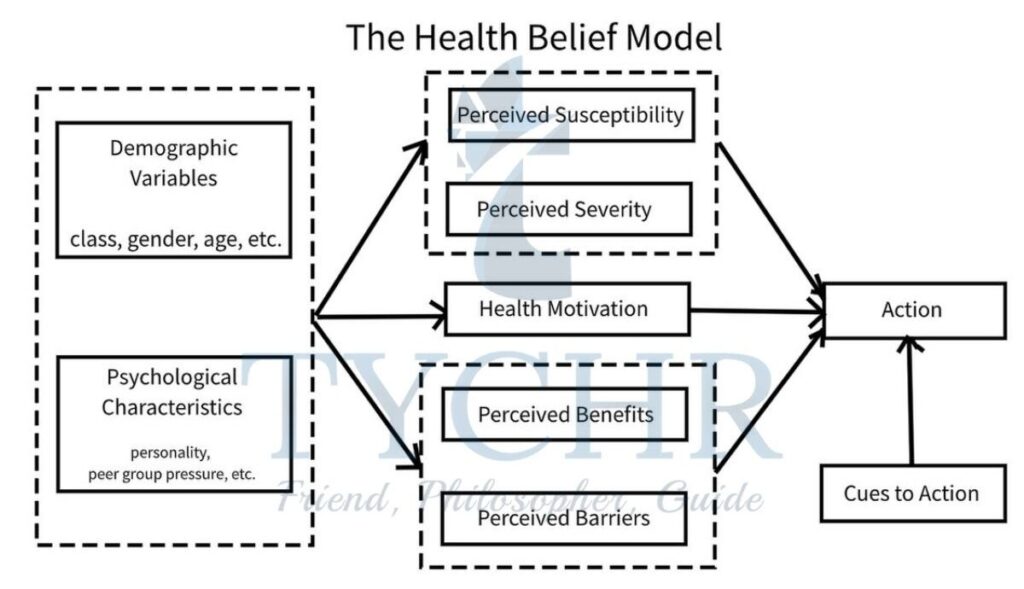
In summary, the HBM suggests that people are likely to follow a given health action if the following apply.
- They think they are susceptible to an illness.
- They think the illness is serious.
- They believe the benefits of the action outweigh the costs.
- They are exposed to triggers for action.
Research done on HBM
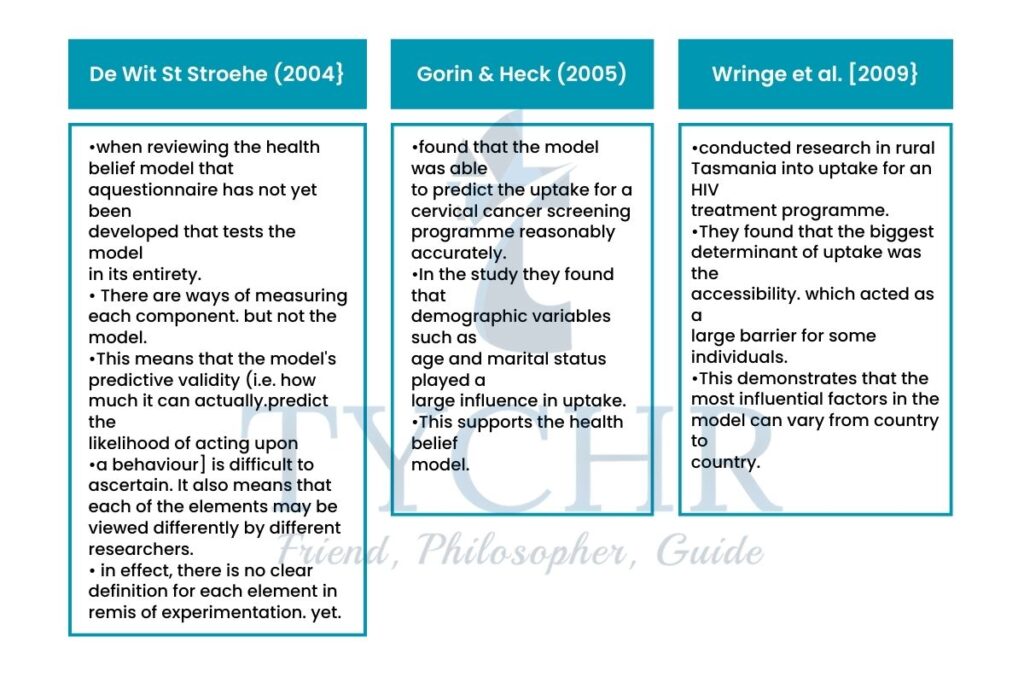
Evaluation of HBM
- There is no account of the emotions involved in the decision-making process. The model acts as if an individual is rational. but decisions are often emotive and there is no evidence of this as a modifying factor. Some researchers argue this is accounted for within the model in the cost/barriers and cues to action section because phobia of hospitals would act as a barrier and the death of a loved one would act as a cue to action. but there is no acknowledgement of emotion as a mediating influence per so.
- The model is argued to be good for explaining individual behaviors such as attending a screening test or having inoculations. It is however not able to explain general attitudes to health. Looking at the development of the model, however. It was designed to examine likelihood of uptake of a behavior so it can be argued that the model is fit for purpose.
- The lack of a questionnaire to measure the model as a whole means that the model has never been tested as a whole entity and this has implications for its validity. However, the model does not claim to calculate the likelihood quantitatively. it is perhaps sufficient that it brings all the various elements involved in decision- making together.
- The research from Wringc er al. {ZCICIQJ above suggests that although the model is cognitive. There is cultural influence on beliefs. Therefore, the model should take this into account and identify where this may occur
THEORY OF PLANNED BEHAVIOUR
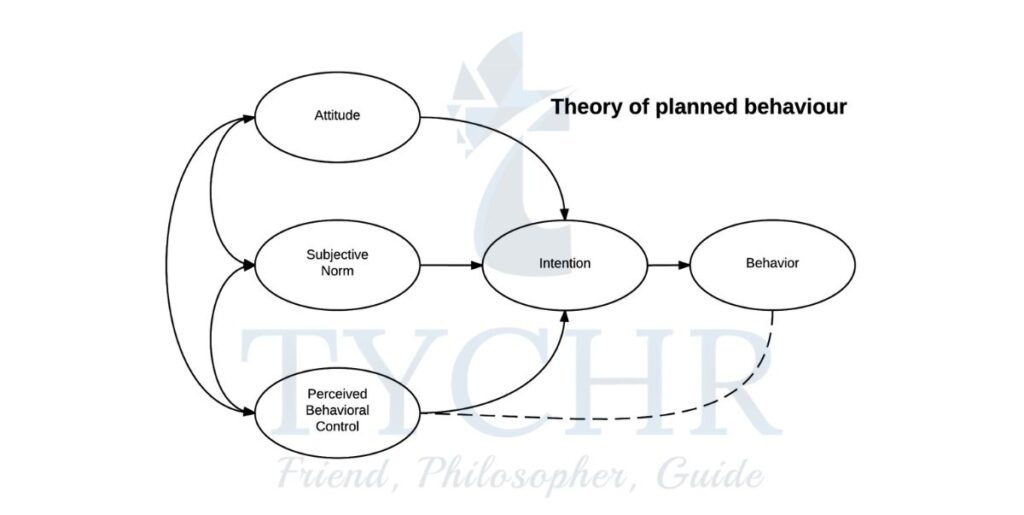
- The theory of planned behavior (TPB) is an attempt to explain why people engage in or avoid certain behaviors. Ajzen developed the theory of planned behavior in 1985. Conner and Sparks (2005) applied this theory to health behavior. Similar to the HBM, the TPB attempts to explain what goes into a decision to engage (or not engage) in a particular behavior.
- We tend to assume that if people intend to do something, then they are likely to do it—but this isn’t always the case. Someone may intend to start eating healthy, nutrient-rich foods but not be able to do so. Perhaps the food is inaccessible or too expensive.
- At best, it seems that if a person intends to do something, he or she will at least attempt to do it. The next question we need to ask is: what factors determine someone’s intention to engage in a behavior?
- The TPB argues it is a combination of attitude, social norms and the amount of control individuals believe they have over the intended behavior
- The core idea of the model is that if we are to predict the outcome of a treatment programme, we need to consider the
beliefs, influences and motivation of an addict to the - There are four parts to the model
1. Attitude
2. Subjective norms and normative beliefs
3. Perceived behavioral control.
4. Behavioral intentions
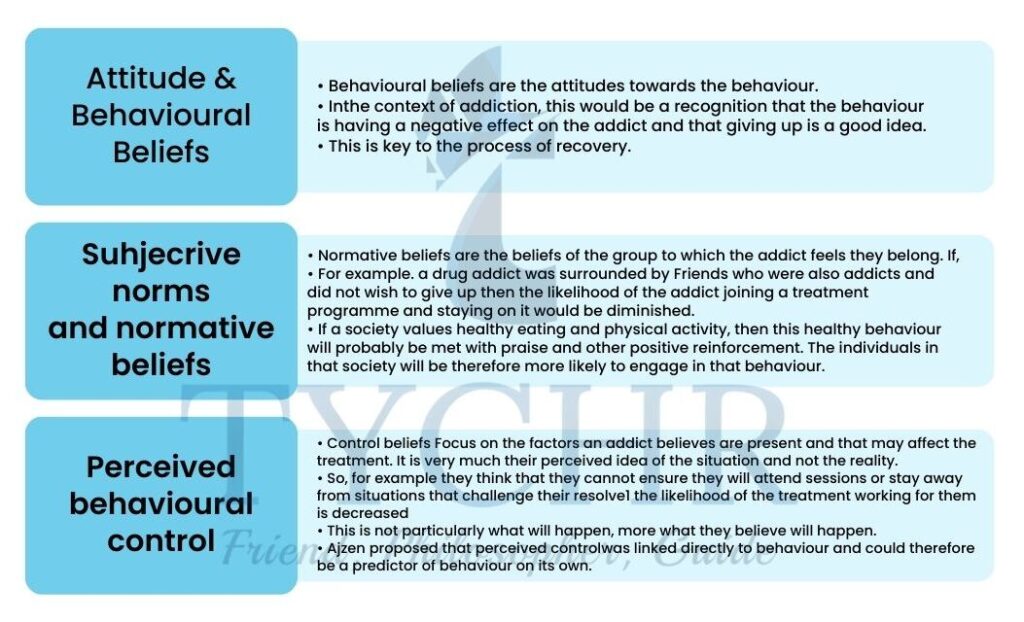
- The theory of planned behavior is used by practitioners to predict the outcomes or potential of treatment programmes.
- They can establish why someone wants to quit and the amount of resolve they have to do so.
- The first section of the model. which focuses on behavioral belier1 is important to ensure they access the treatment initially.
- The second stage of normative beliefs ensures that social support is present and that negative peer and family influence can be dealt with.
- The final section of perceived control is a good indicator for the success of the programme.
- If an addict does not believe that they can stop their addictive behavior, For example by stopping gambling or giving up smoking, it is unlikely that they will do
Research done on TPB
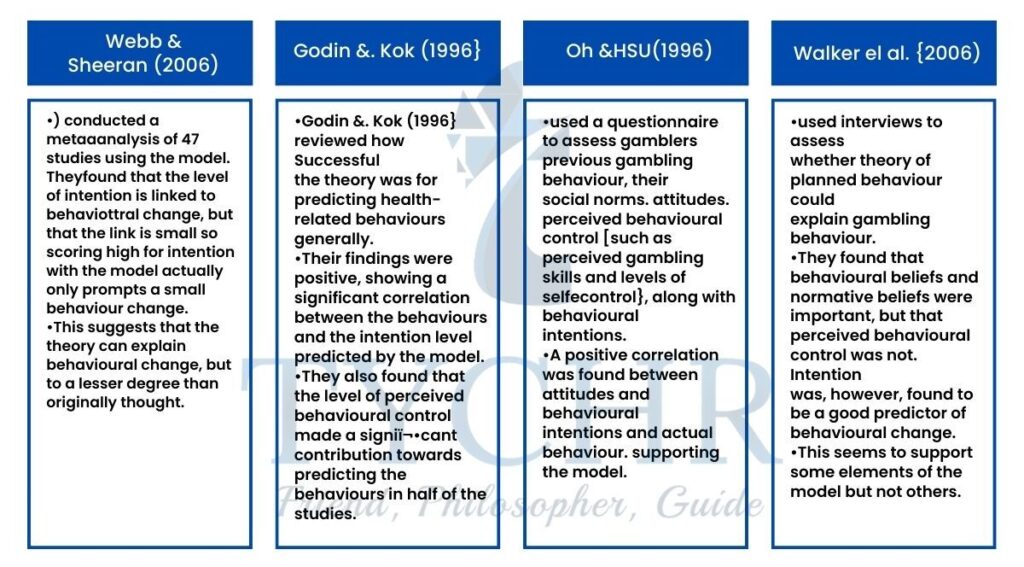
Evaluation
- The theory is used widely in health psychology and health economies This suggests that practitioners acknowledge its validity and deem its predictive power as useful.
- Emotions are not considered in this model which causes an impact on the likelihood of a change in behavior. Addiction is one of the examples for this, where a person’s state is endangered by mood.
- A strength of the model is its accepting the roles of peers in an influencing manner. This influence never stops once the behavior is developed and therefore should be kept in mind while making a prediction about the outcomes of the behavior changing programs.
- The model relies on self-report measures to gauge its effectiveness. This is a potential problem as the participants could be irrational and liable to downplay the level of their addiction. This means that the effectiveness measures may be unreliable
- The practical application of this model is one of its strengths. Practitioners can use it to decide whether an intervention will be effective, and as such, time and money are not spent if it is not going to be effective for the individual.
Module 5.4: Dispositional factors and Addiction
What will you learn in this module ?
- Dispositional factors
- Addiction
Dispositional Factors
- Dispositional factors are internal factors that affect health and are characteristics of an individual. They can include anything from genetics to personality and are mostly indirect and out of the individual’s control (to some extent) but this does not make them any less important.
- Genetic vulnerability and personality are considered with regard to health behavior below.
- This section looKs specifically at addiction. Probably the best way to describe addiction is to refer to the diagnostic manual to see what is now defined as dependence. This varies depending on whether it is dependence on substance [like nicotine} or behavioral {like gambling).
- Alcohol is given separate diagnostic criteria. which are similar to substance-related addiction.
- There is a list of all symptoms of which two need to be evident for diagnosis to be made. They also need to be present together in the same period. Examples of the indicators are:
- taking the substance in larger amounts or for longer than intended
- anting to cut down or stop using the substance but not being able to.
- Giving in an ample amount of time gets out of the usage of the substance.
- Desire or the sudden urge to use the substance.
- Unable to manage what you should do at work/home or school because of substance use.
1) Genetic vulnerability
- There is thought to be a genetic influence on development of addiction, much like many other behaviors.
- Nielsen et al. [2009} compared DNA from former heroin addicts and non addicts and they found a connection between the genetics of the individual and their genetic make-up.
- However, it is absolutely necessary for there to be a gene-environment interaction for this to occur. The individual will plainly not become addicted if they are not exposed to the substance or the opportunity within their environment.
- Therefore, genetic vulnerability should be seen as an interaction.
- Twin studies have been useful for picking up on a heritability component to addiction. So too have linkage studies of addiction to substances and genetic make-up.
- These have shown an association between genes and: 1} alcohol {Foroud at al., ZDUOl; 2} nicotine {Li et al., 2(104}and 3) cocaine {Gelernten 2.005}.
- For.eg
In the case of alcohol1 the way the genetic code affects the likelihood of addiction is the way in which alcohol is metabolized by the body. The first reaction of our body to alcohol is to metabolize it to acetaldehyde then to acetic acid. The acid is released into our urine very quickly. Otherwise we can feel nauseous. In about 50 percent of people from Asia. their genetic code does not facilitate the release of the acetic acid into the urine so they feel nauseous when drinking alcohol. Clearly this means their chance of addiction is slim to none.
2) Personality
- It is argued that people who have pathological personalities are more likely to become addicts because the drug or behavior they are addicted to initially offers them relief.
- Pathological personalities are types that have a predominantly negative persona. Their personality means they may be more stressed and find life difficult.
- The temporary high gained from playing a fruit machine or drinking a vodka and tonic, for example, would make them more likely to keep doing it.
- This means ultimately that the personality triggers the addiction rather than the other way round.
3) Addictive personality
- Various theorists have proposed the existence of an addictive personality. Eysenek (1991) outlined a model that suggested addictions occur because of personality type and the needs of the personality. He argued that those with high neuroticism levels were predisposed to addictions.
- Neuroticism is characterized by high levels of anxiety and irritability. He also added that high levels of psychoticism were linked to addiction because this meant that the individual was aggressive and emotionally detached, so the high associated with drugs or certain behaviors helped this.
- Eysenck also argued that there was a biological basis to personality and therefore the personality was inherited. Following this argument through. it would seem to suggest that someone is born with a predisposition to their personality.
- Novelty seeking is the need for change and stimulation. Individuals will actively seek new environments and experience, almost as if they have a low boredom threshold.
- This element makes them more likely to seek out sensations from drugs.
- Harm avoidance is the amount that a person worries and sees the negative elements of a situation. This can affect their likelihood of taking a drug and therefore becoming addicted to it.
- Cloninger’s theory suggests that addiction occurs in individuals with a low level of harm avoidance.
- Reward dependence in an individual is when someone reacts and learns from a rewarding situation quickly. This also predisposes them to addiction. as the rewarding effects are experienced quickly and easily
4) Stress
- It is easy to see why high levels of stress would make you more vulnerable to addiction.
- Turning to behaviors and drugs that give a temporary relief from stress is a type of coping mechanism.
- Stress can be short term or long term and it is the long-term exposure to stress that could increase the likelihood of someone being addicted.
5) Family influences
- There are two key ways that families can leave an impact on addictive behavior: social pedagogy and anticipation.
- They can either put an individual at risk of addiction or protect them to some extent from developing addictive behavior.
- Social learning is the learning of behavior by observation of role models in the
- environment. If the individual sees that model rewarded for their behavior then the vicarious reinforcement is going to increase the likelihood of the observer imitating the behavior.
- It is clear how that could occur with addictive substances within a family.
- However it should be noted that the addiction is not the imitated behavior; it is the desire to try the substance that is the influence.
6) Peers
- Given that social influence is often seen as the psychological explanation for initiation to addictive behaviors, the influence of peers is potentially great.
- However, as with many of the vulnerability factors proving causation is problematic.
- It is just as possible that choice of peer groups is influenced by addiction.
- So an addict might choose a peer group that allows them easy access to the focus of the addiction {e.g. drug) and they may choose a non-judgemental peer group.
- Peers are influential at the intervention stage1 too, as they can provide access to drugs and may encourage a relapse.
- It is argued that these social influences should be considered when making and delivering an intervention programme to try to ensure maximum success levels.
7) Brain neurochemistry: the role of dopamine
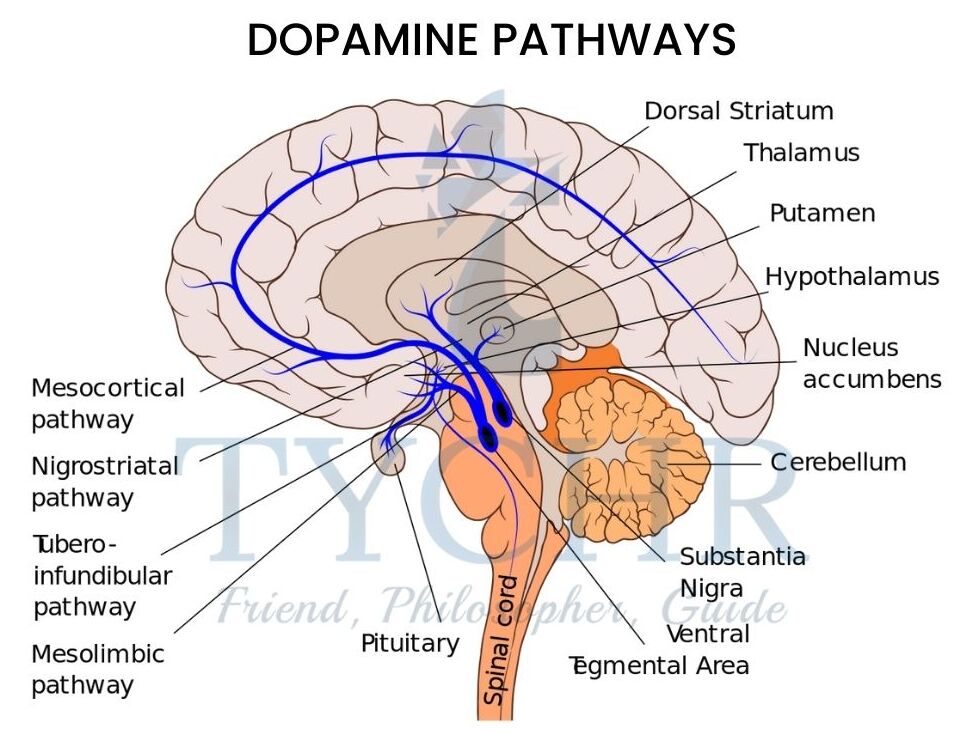
- Dopamine is implicated in addiction as the addictive substance or behavior prompts a high through boosting the activity of the brain’s reward system.
- This system is found in the center of the brain and is a complex circuit of neurons that produces a high, like euphoria, which means the individual is tempted to take the drug again or repeat the behavior.
- The brain mechanism is basically a pathway of neurons that is activated by the neurotransmitter dopamine. The source of the activation is the ventral tegmental area {VTA},which has many dopamine neurons. This then triggers activation in the limbic system {specifically the nucleus} and this subsequently boosts activity in the prefrontal cortex.
- This activity is called the “common reward pathway”,
as it is associated with the feeling of euphoria. - As time goes on, and through repeated usage, the level of drug needed to elicit the reaction becomes greater.
- This occurs due to a change in the neuronal structure in the pathway which accounts for tolerance levels increasing in an individual and also why the individual craves the drug or wishe
to carry out the behavior. - Addiction is the result.
Module 5.5: Promoting health

What will you learn in this section?
- Approaches to health
- promotion Population health
- approach Individual health approach
- How to make health promotions effective
- Education and cognitive dissonance (Festinger, 1957)
- Fear appeals work best with strong selfefficacy messages (Witte and Allen, 2000): Legislation, subsidies, and taxation
Health promotion often uses a holistic population health approach. This approach focuses on improving health through policies that affect the health of an entire population, rather than individuals. Throughout the 20th century, states have been taking a larger and larger role in influencing the health of their populations.
Political leaders realized over the past century that a healthy working population was essential to a growing economy, so health promotion became a top priority for both developing and developed nations..
- In an attempt to encourage good health globally. the World Health Organisation has defined five key principles to outline the areas that health promotion should consider:
- The general population as a whole should be considered for health promotion, not just specific target groups who could contract specific diseases.
- The promotion should be focused on the cause of the health problem, including the individual’s environment.
- Health promotion should be a combination of complementary methods and a variety of communication mediums he should use.
- Promotion should try to include public participation and encourage the formation of self-help groups.
- Health professionals should be consulted and involved in health promotions.
These principles clearly acknowledge the role of the health professional,the individual and the social and environmental factors in the good health of the global population.
The approaches of health promotion
Self-empowerment approach

- This approach focuses on the control of the individual over their body and the environment.
- It is likely that adherence to the program and thus its success will be increased if the individual affected feels they have some control over the outcome, which means they will also be more likely to do something about their health.
- This means taKing a less prescriptive approach and encouraging individuals to make lifestyle choices that will impact on their general health.
- A good example of such an approach is the “This Girl Can” campaign, which aims to address the issue of low sports participation numbers in Women.
- Fear of judgment was identified as a barrier to women taking part in sports owing to being concerned about their appearance, thinking they are not good at sport and prioritizing others over themselves.
- The campaign was designed to address those fears in women directly, and it is used as a film of real women exercising together with slogans such as
˜sweating like a pigs”.
feeling like a fox”.
“l jiggle therefore I am” and “I kick halls, deal with it”
Community development approach

- The community development approach is just that health promotion within the community so that the environment of the individual changes and social support is available
- Self Help groups are an example of this kind oi” health promotion.
- In Beijing, China there is a landmark known as the Temple of Heaven. Every morning large numbers of retired people gather in the grounds to do some form of activity together in groups.
- Tai chi, choirs and line dancing, among other activities. are on offer.
- It is apparent to visitors that there is a strong sense of community and support. It promotes activity and companionship which supports good health.
Behavior change approach
- This approach to health focuses on the cognitive level.
- People hold beliefs that are not realistic. These are particularly damaging from a health perspective, where faulty thinking causes an individual to feel they are not at risk of poor health or a specific disease.
- A public health campaign can address that misperception by presenting facts and highlighting who might be at risk. There are ways of doing this.
- For example, message content has been shown to be more effective if both sides of the
- arguments are given. The individual receiving the message retains an element of control, which makes it more attractive.
- Another way is to present information including statistics that can be perceived in several ways by an individual; so if. for example, you say the risk of disease is a 10 percent. This can be seen either as risky or minimal depending on the contest.
- Health promotion campaigns using this approach are designed to change the individual’s way of thinking about their health. This can be done in a variety of different ways, for example by giving facts and the reality of the. situation so that they do not hold misperceptions that they are not affected.
- An example. This approach was the one taken to challenge the idea that heart disease.only affected men. It was designed by the British Heart Foundation and involved erecting temporary cardboard gravestones in five UK cities. The gravestones had words such as ‘Mum And “Grandma” written on them to raise awareness of potential female fatalities
from heart-disease related problems. This campaign also aimed to raise money which it did. over £1 million. - The AIDS campaign of the 1980s also used shock images to raise awareness of the condition.
- At that point there were no known treatments so the diagnosis was a death sentence.
- Prior to the campaign the disease was seen as affecting homosexuals, so the government wanted to address that misperception.
- The campaign image was striking in that it emphasized the terminal
prognosis for that time. With gravestones, flowers and black and white images.
Tools of health promotion
1) Education
- Because individuals must first comprehend the repercussions of a behavior in order to comprehend the necessity of change, education is an essential component of health campaigns.
- For instance, convincing people that smoking tobacco causes a number of terminal cancers and cardiovascular diseases is necessary for changing people’s attitudes and beliefs about smoking.
- Cognitive dissonance theory, first proposed by Leon Festinger in 1957, is the central concept behind education as a preventative factor. Cognitive dissonance theory is founded on three fundamental tenets.
When their beliefs and actions diverge, people are aware of it.

- These inconsistencies make people uncomfortable.
- People will try to align their actions with their beliefs.
- they can do this in three ways: change their beliefs, change their actions or rationalize their irrational actions.
- The statements “I smoke a pack of cigarettes every day” and “smoking tobacco will give me lung cancer and kill me” are two examples of this kind of psychological inconsistency. Holding these two thoughts in your mind simultaneously causes distress. Smoking can be stopped, a person can change their mind about how dangerous it is, or they can justify why they smoke. It turns out that people are very good at justifying irrational behavior.
- The point of education in health promotion campaigns is to create cognitive dissonance by influencing an individual’s beliefs about a certain behavior.
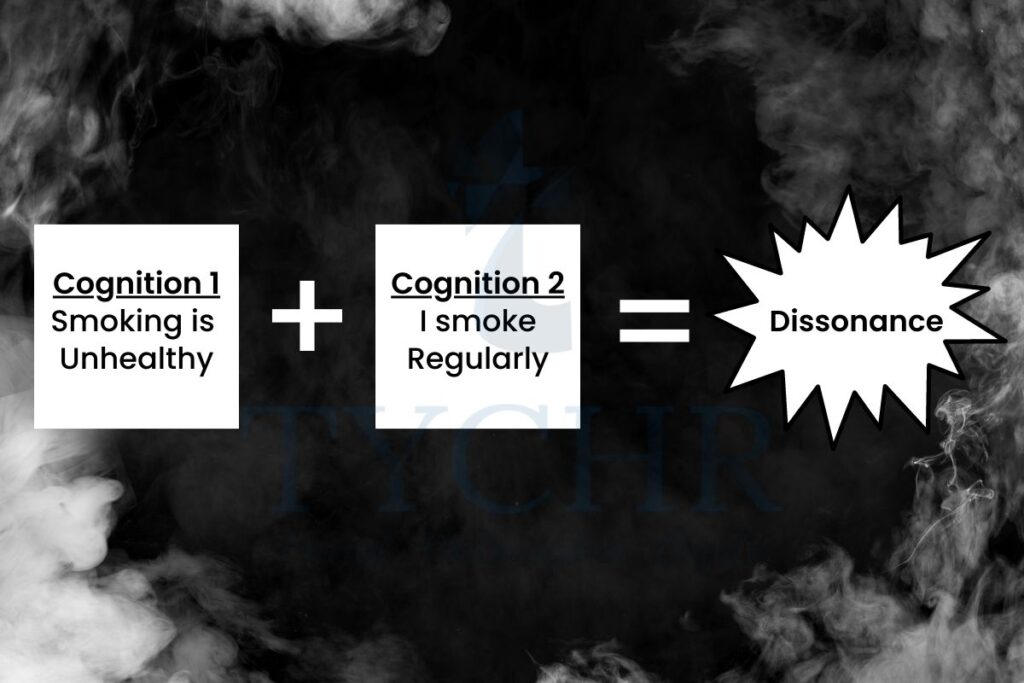
- It is more likely that a person will need to change a behavior in order to overcome the cognitive dissonance if it is possible to convince them that the behavior in question is unhealthy.
2) Fear
- Health promotion relies heavily on fear appeals and education.
- Fear appeals “are convincing messages that stress on the danger and cause harm that could cause to the people if they do not follow the messages. recommendations”(Albarracin, 2015).
- According to Witte and Allen’s (2000) metaanalysis of fear appeal campaigns, strong self-efficacy messages must accompany fear appeals in order for fear to be a powerful health behavior motivator. “If fear appeals are disseminated without an efficacy message, they run the risk of backfiring, since they may produce defensive responses in people with low-efficacy perceptions,” they write.
- Self-efficacy is clearly an essential component of any fear appeal.
- On various samples, fear appeals performed differently. For instance, they were more successful in samples with all female participants and Asian participants.
- Last but not least, Tannenbaum discovered that ongoing behaviors like dieting and exercise were more susceptible to fear appeals than one-time-only behaviors like health screenings.
3) Legislation and health problems
- Additionally, legislation enacted by the government frequently encourages healthy behaviors.
This extends beyond taxation and subsidies, such as food labels, consumption restrictions based on age, and sales restrictions based on geographic location. - Numerous government and agency interventions in the area of food labeling are expanding. The thought is that the idea of mental discord is brought to the item level.
- Every time a product is displayed to a customer, they are reminded of the potential side effects that could have on their health.
- The consumer’s education and interest determine
- the effectiveness of nutrition and food labeling. The Food and Drug Administration of the United States, formerly known as the FDA, recently modified their food labeling policy in an effort to incorporate the most recent scientific information, such as the connection between diet and chronic non-communicable diseases.
- According to the TPB and HBM, this intervention aims to alter attitudes and, as a result, to address the cognitive determinant of obesity.
4) Taxation and Subsidies
- Some risk factors necessitate society-wide solutions on a large scale.
- A report titled “Deficit financing for Diet and Prevention of Noncommunicable Diseases” was recently published by the World Health Organization (WHO, 2016).
- In order to encourage responsible and healthy eating, this report urges nations to impose taxes on food and provide subsidies for its purchase.
- The report contends that rising the cost of sugar improved drinks, appropriations on the cost of new products of the soil, and designated tax assessment on unfortunate food varieties will bring about superior populace wellbeing
- A special reward to this sort of activity is that the assets raised through tax assessment can be put toward the expenses of carrying out training programs encompassing weight or in assisting with paying for the sponsoring of better food choices
Module 5.6
Health problem 2: stress
What will you learn in this module?
- Definitions of stress
- Theories and models of stress
- Models of stress
- Promoting Health
- Definitions of stress
“If the problem has a solution, why stress yourself?
“Stressing yourself won’t do any good if the problem has no solution .” (Shantideva) - Stress has been shown to be both a health and wellness determinant and a risk factor for obesity, substance abuse, and numerous non-communicable diseases. Stress, obesity, and substance abuse are all intertwined in a complicated way.
- Because “stress” means different things to different people, it’s hard to define. We frequently apply the term to any circumstance that makes us feel helpless, angry, upset, or agitated, overgeneralizing it. At this point, it is essential to introduce and differentiate a few related ideas that we will use throughout this chapter. We will rely on Robert Sapolsky for assistance. In order to comprehend the nature of stress, Sapolsky contends that it is essential to distinguish between psychological and social stressors, acute physical stressors, and chronic physical stressors (both of which are biological approaches to defining stressors).
- Acute physical stressors are those events that are extremely demanding but only last a short time and force your body to use its energy reserves to help you deal with the situation. If you were in the same situation as fleeing an irate lion, your stress response—the “fight or flight” response—will aid in your survival. Examples that are more typical for humans include going to the dentist or having a wasp enter your vehicle while you’re driving (Elliott and Eisdorfer, 1982; Hobfoll,1989). While the stressor will soon pass and your system will return to its normal balance, you may feel the stress response (increased heart rate, sweaty palms, etc.) in these situations. We refer to this equilibrium state as homeostasis. The idea of homeostasis alludes to the thought that the body needs equilibrium, and we have an optimal degree of glucose, oxygen, temperature, etc that we really want to keep up with assuming our bodies are to work at their best.
- Chronic physical stressors require the body to prepare for a long-term physical challenge, such as fighting a parasite or walking miles to find food. The stressor has a long-term physical effect on the body, but humans are pretty good at handling these demands. Our bodies frequently have the ability to return to a state of homeostasis once these demands are met.
- psychological and social stressors are normal in our day to day existence and as people we are fit for making or envisioning distressing occasions that can attack our considerations for days, weeks or months all at once. When we are stuck in traffic, worried about an upcoming event, or thinking about a conversation we had with our boss, we can experience stress. The body’s stress response is continually triggered by these psychological stressors over time. This prolonged activation of the stress response in our bodies can cause illness and injury.In their explanation of the primary types of stressors,
- Elliott and Eisdorfer (1982) include the chronic and intermittent stressors.These may include examinations and regular meetings with teachers who you don’t like.
- Simply put, a stressor is anything that upsets your body’s homeostatic equilibrium (Sapolsky, 2009), and strain is the mental and physical response to that stressor (Sarafino, 2017). Stressor can be both positive and negative. As a result, we will use the definition from the beginning of the section:
“stress is any uncomfortable emotional experience accompanied by predictable biochemical, physiological and behavioral changes” (Baum,1990).
Models of stress
1. A sociocultural approach to stress
- Our daily lives are full of stresses and strains. From the moment that our alarm clocks sound to wake us in the morning until the moment that we go to bed at night, our days are filled with events that we find psychologically and physiologically stressful.
RESEARCH
- Holmes and Rahe (1967) conducted a classic study with over 5,000 participants who made a list of stressful life events. These occurrences, both positive and negative, were frequently unanticipated. The researchers gave marriage an arbitrary value of 50, and they asked a new group of participants to rate each alternative to marriage in terms of how much adjustment it would require to their lives (Morrison and Bennett, 2016). A score of 100 would be given to events that are perceived to be twice as disruptive as marriage. The scores for these events, which ranged from 11 to 100, were then ranked.
- This was known as a life-changing unit score (LCU). The highest level of adjustment was found to be to the death of a spouse. Holmes and Rahe hypothesized that the more life events an individual had experienced within a one-year period, the more likely they would be to suffer from stress-related illness. Participants gaining a score below 150 were not reported as suffering from stress.
- Participants scoring over 200 were seen as suffering from severe stress and at risk of stress-related illness.
- In contrast to Holmes and Rahe’s major life events theory, Kanner et al (1981) proposed that it was in fact the small, seemingly harmless, day-to-day occurrences which they termed “daily hassles” that were in fact causing us stress. They argue that daily hassles such as being stuck in a traffic jam or losing your phone could have a detrimental effect on our health if they are not experienced alongside an equal measure of positive occurrences.
- They termed these positive experiences “uplifts” and these include something as simple as getting a good night’s sleep, receiving praise from a teacher or having an enjoyable first date. These uplifts have been studied in their own right by Lazarus and his colleagues and they found that positive experiences can indeed improve our overall sense of health and wellness.
- Lazarus, Kanner and Folkman (1980) argue that positive events can act as a buffer to the negative events, providing some respite and therefore reducing the impact of the stressful daily hassles. McLean (1976) highlights the importance of investigating the occurrence of both negative and positive events together: “Perhaps because the unit of stress is relatively small and the stressors so familiar, these kinds of stressors have taken advantage and are regarded less prominent than more stressors which are dramatic.. Clinical and research data indicate that these ‘microstressors’, acting cumulatively, and in the relative absence of compensatory positive experience, can be potent sources of stress.”
- In their classic study, Kanner et al (1981) wanted to compare the impact of daily inconvenience and boosts as predictors of psychological symptoms of stress with major life events as proposed by Holmes and Rahe. Over a period of 12 months, they studied 100 participants, primarily from California, USA, using both psychometric and self-report measures. Participants received the surveys one month before the start of the study to ensure all had received and understood the materials. They recorded their experiences using the following measures:
- the hassles and uplifts scale consisting of a possible 117 hassles and 135 uplifts which they rated for frequency of occurrence and intensity
- a life events scale
- the Hopkins Symptom Checklist
- the Bradburn Morale Scale (the last two tests for psychological well-being in adults). Results showed that daily hassles were in fact stronger predictors of psychological symptoms of stress than life events.
2. Cognitive Approach To Stress
Transactional stress model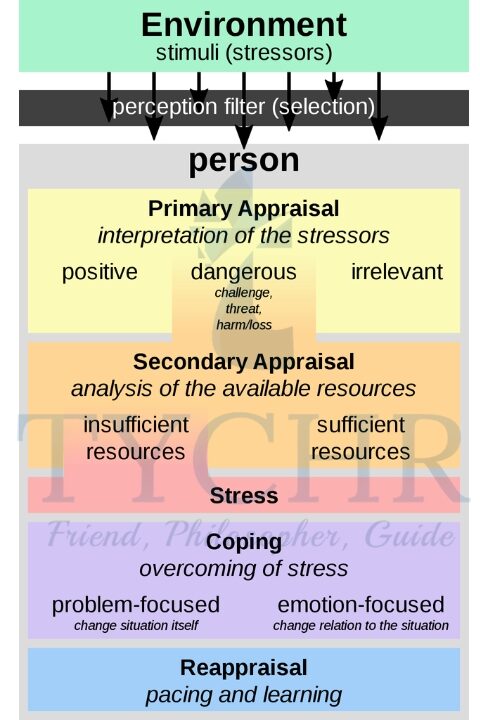
- In the 1970s, Richard Lazarus and his colleagues argued that stress was the result of interactions between people and their surroundings.
- They argued that stressors are perceived as threats, challenges, and potential harm. Additionally, people evaluate their capacity to deal with these stressors in relation to the resources available to them.
- According to the transactional stress model, an individual will engage in either primary or secondary appraisals when confronted with a stressor.
- a) In primary appraisal we interpret the potential impact of the current situation on our well being. We ask ourselves questions such as, “What does this mean for me?” and “Could this stressor hurt me?” Lazarus and Folkman suggest four ways to appraise such events:
- irrelevant (this does not concern me)
- benign and positive (this is good)
- harmful and a threat
- harmful and a challenge
- b) Those situations that we do appraise as stressful undergo the process of secondary appraisal in which we consider our potential to cope with a situation by using the resources available to us. For example, individuals with alot of insecurity are more likely to have low self-esteem and may be more likely to assess a situation as stressful as they think they do not possess the help needed. A final reappraisal of the situation is undertaken in light of our own responses to the stressor and the information available.
- a) In primary appraisal we interpret the potential impact of the current situation on our well being. We ask ourselves questions such as, “What does this mean for me?” and “Could this stressor hurt me?” Lazarus and Folkman suggest four ways to appraise such events:
RESEARCH
- Speisman et al. (1964) conducted a classic study that appears to support the transactional model of stress. Boys who reported on their own levels of stress watched a stressful movie about a tribal genital mutilation ritual. The researchers took measurements of their skin conductance and heart rate.
- Members were put into one of four circumstances:
- The control condition had no soundtrack; the trauma condition had a soundtrack that emphasized the danger and pain of the ritual; the denial condition had a soundtrack that was intended to provide an objective, “scientific” account of events; and the science condition had a soundtrack that emphasized the boys’ consent to participate.
- Speisman et al. (1964) conducted a classic study that appears to support the transactional model of stress. Boys who reported on their own levels of stress watched a stressful movie about a tribal genital mutilation ritual. The researchers took measurements of their skin conductance and heart rate.
- Members were put into one of four circumstances:
- The control condition had no soundtrack; the trauma condition had a soundtrack that emphasized the danger and pain of the ritual; the denial condition had a soundtrack that was intended to provide an objective, “scientific” account of events; and the science condition had a soundtrack that emphasized the boys’ consent to participate.
- Results showed that participants in condition 2 (the trauma condition) experienced more stress than participants in the other conditions, demonstrated by their self-reports, increased heart rates and skin conductance.
- The appraisal of the video as traumatic and painful influenced the participants’ subsequent
- primary appraisal of events. The study highlights how it is our interpretation of an event that can cause an emotional response, that two people can perceive and appraise the same stressor differently, and that this will trigger differences in their stress response. It is therefore possible for purely psychological factors to increase or decrease the biological stress response.
3. The Conservation Resource Model
- Hobfoll (1989) introduced a new alternative model of stress, the conservation of resources model. The model’s
basic proposition that people try to retain , to retain, defend and construct resources and the feeling of stress or when they feel they have lost their connection with the resources (Hobfoll, Briggs-Phillips and Stones, 1989). In order to make sense of this model we must once more adapt our definition of stress.
Hobfoll defines psychological stress as a response n to the surrounding in which there is one of the following:- the threat of a net loss of resources
- the net loss of resources
- Less resource get following the investment
of resources.
- Perceived loss, actual loss or lack of gain in resources are sufficient to produce psychological stress. In order to understand this theory we must first understand what is meant by “resources”. Resources are any object, characteristic or condition valued by the individual. These include social support, self-esteem and employment (Parry, 1986).
- An example of loss of resources may include a demotion at work, unemployment or divorce. These environmental resources are particularly important as not only are they functional—they provide financial support or security—but they also help people de ne their sense of self, and any loss would threaten their self-esteem.
4. Integrated Approach to Stress
- The typical worker will work 39 hours per week. We devote a significant amount of time and emotion to it, making it an essential part of our day-to-day lives. As a result, it’s critical that we enjoy our jobs.
- According to Patrick Lencioni (2015), genuine engagement is necessary for our happiness at work. He argues that the following factors can contribute to workplace misery:
- Work engagement can be defined as a positive, satisfying, and attentive state of mind that is primarily characterized by:
- anonymity (the feeling that you are invisible or that people do not know you)
- irrelevance (the feeling that your job doesn’t matter)
- immeasurement vigor—having a high level of energy and resilience in relation to one’s work dedication—having a sense of significance, pride, and enthusiasm—being completely engaged in one’s work
- Circumstances at work that are not connected with this could cause pressure. According to the Centre for Studies on Human Stress, there are four common causes of stress.
- Novelty: something brand-new that you’ve never seen before
- Unconventionality — something happens that you had absolutely no chance of knowing would happen.
- Threat to the ego—your personal competence is questioned.
- a sense of control—the impression that you have little or no control over the situation.
5. Biological Approach to stress
- These real-life examples of stress make it clear that our cognitions have the potential to alter our physiology, that is, our appraisal of events as stressful has the potential to activate a biological response.
- Walter Cannon (1932) termed this response the “fight or flight” response. When exposed to a stressor such as coming face to face with a bully, our body immediately attempts to deal with the threat by entering a higher state of arousal. Most of us will be familiar with this feeling: increased heart rate, pupils dilating and body shaking. Your body has prepared itself to deal with the threat by making use of all available resources allowing us to summon the energy to either fight or run away.
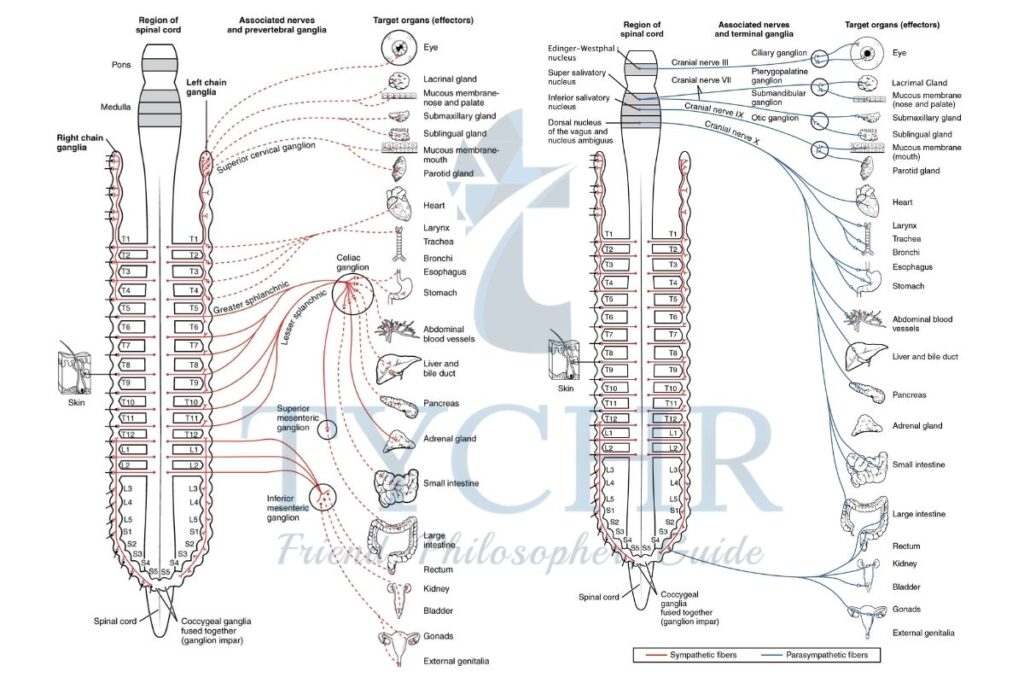
Stress and autonomic nervous system - The nervous system acts as the body’s communication center, relaying information about internal and external
conditions to our brain. There are two parts of the nervous system :- The central and
- peripheral nervous system
The central and the peripheral nervous systems consist of neurons that are involved in the process of neurotransmission,
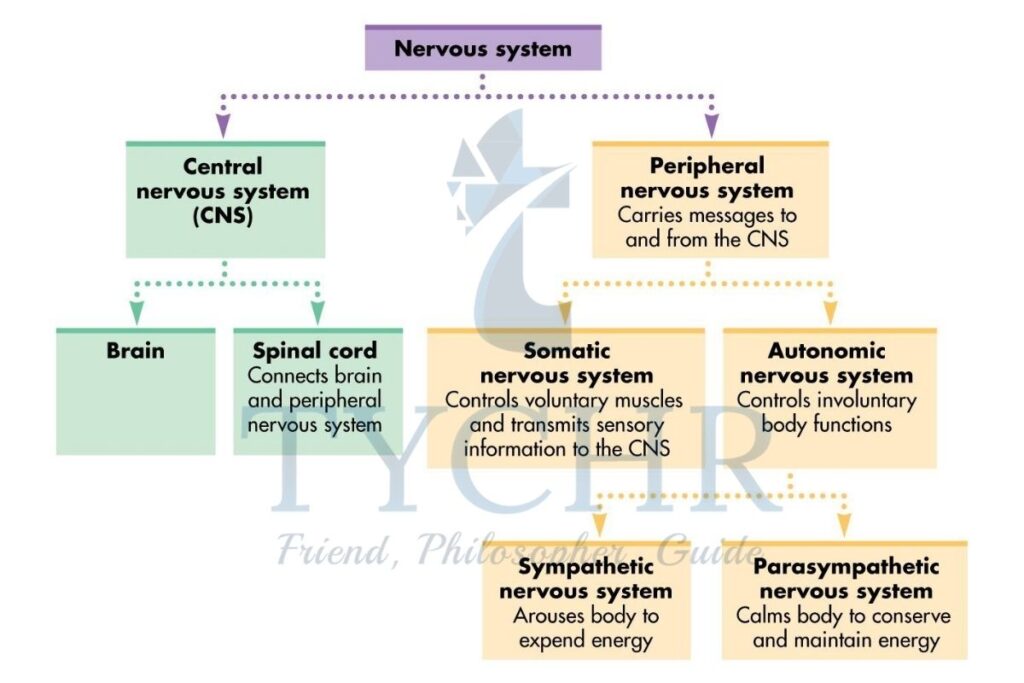
- The sympathetic nervous system is activated during states of emergency, real or imagined. It helps ensure that we are the challenge to our system by heightening arousal, vigilance and mobility. It means you have the strength and energy needed to deal with that bully—fight or flight. When this system is activated your adrenal glands secrete adrenaline (epinephrine) and noradrenaline (norepinephrine). It is the adrenaline rushing around your body that causes you to experience an increased heart rate or shaky hands.
- While the parasympathetic nervous system calms things down. The parasympathetic nervous system mediates calmer activities such as digestion and growth.
- The two systems work in opposition to each other. While you are preparing to fight, or more sensibly run away from that bully, activating your sympathetic nervous system, your reproductive systems shut down as they are not needed and the energy is mobilized elsewhere.
- The sympathetic and parasympathetic nervous systems cannot be switched on at the same time, so the functions of each are inhibited when their counterpart is active. As a result, our body does not respond well to prolonged exposure to the stress response as we neglect other essential functions such as fighting infection.
Stress and Hormone
- Your body begins to secrete stress hormones when you experience or even perceive a stressful event: The sympathetic nervous system produces adrenaline and noradrenaline, as well as glucocorticoids, which are steroid hormones produced by the adrenal glands.
- Cortisol, also known as the stress hormone, is the most widely used glucocorticoid. The stress response is caused by glucocorticoids and secretions from the sympathetic nervous system working together.
- When we evaluate an event as stressful, the brain initiates this hormone secretion process. Corticotropin, which is produced by the hypothalamus, directs the pituitary gland to produce the hormone ACTH.
- When ACTH reaches the adrenal glands, it causes the production of glucocorticoids, which in turn causes the stress response to be triggered. This framework is frequently alluded to as the hypothalamic-pituitary adrenal pivot (HPA)
The General Adaptation Filter
- Hans Selye wrote in 1951, “Unless it is met by adequate adaptive responses, anything that causes stress endangers life.” On the other hand, anything that puts one’s life in jeopardy elicits responses that are both stressful and adaptive.
- Therefore, adaptability and resilience to stress are necessary for survival. Selye asserts that the biological term for stress is “stress,” and that all living things respond to stress in the same way.
- The first study to document the negative effects of stress on the human body was Selye’s. He named this versatile reaction to push the overall transformation condition. He came to the conclusion that prolonged stress will cause illness when he realized that the rats he had been using for his research had developed stress-related illnesses despite the experimental conditions they had been placed in.
- Selye had repeatedly injected these rats with a variety of substances and handled them carelessly. He concluded that the rats’ fear of being injected was the root cause of their recurrent stress response activation. As a result of their prolonged exposure to the fight or flight response, the rats’ bodies were flooded with stress hormones, eventually leading to stress-related illnesses.
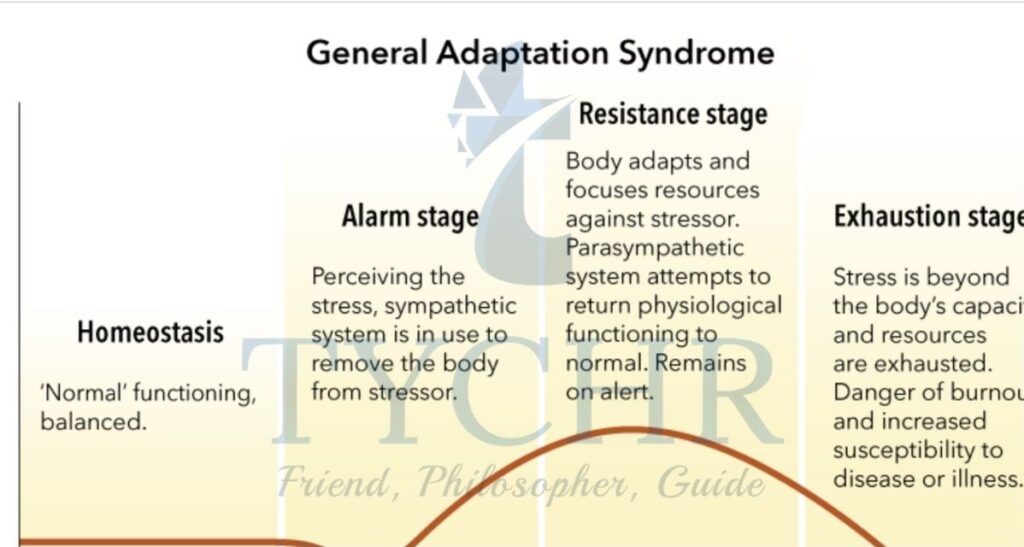
- The general adaptation syndrome consists of three stages.
1. When the body is put under stress, the fight or flight response kicks in, allowing it to gather the resources it needs to survive.
2. When the body actively fights back against a stressor that keeps coming up, this is the stage of resistance, which keeps the stress response going.
3. The point where the body’s resources run out and it is unable to deal with the stress response is known as the stage of exhaustion. Presently we are probably going to become ill. - The research conducted by Selye found that, regardless of the stressor, the body will always respond to stress in the same way, and that prolonged exposure to the stress response can result in illness.
- But it’s important to remember that not all stress is bad.
Humans can actually enjoy stress when we have the right amount of it. - Positive stress, such as feeling nervous before a race, was referred to by Selye as eustress. Negative pressure is known as pain. Selye was of the opinion that eustress and distress had the same response, and that eustress would eventually transform into distress if the stressor got more intense.
- This connection between arousal and performance was the goal of the Yerkes-Dodson law. Performance would be supported by a certain level of arousal, but if this level was exceeded, performance would suffer.
Promoting Health
- Physical activity can be an effective buffer against stress. This may seem paradoxical because exercise increases levels of circulating cortisol, the so-called stress hormone. Exercise improves your overall health and well-being and triggers the release of endorphins and noradrenaline.
- Endorphins are related to pain reduction and act similarly to drugs such as codeine and morphine. Despite the widely accepted belief that exercise reduces stress, the mechanisms through which exercise reduces stress are still not fully understood.
- Additionally, yoga is an effective stress reliever. Yoga is a popular form of relaxation and well-being that incorporates specific postures, simple meditation, and breath control. It has roots in ancient eastern practices, like mindfulness. Pascoe and Bauer (2015) played out an orderly survey of studies looking at the impacts of yoga on the thoughtful sensory system and hypothalamic-pituitary-adrenal pivot (HPA). They looked at 25 randomized control studies and found preliminary evidence that yoga can improve the movement of the hypothalamic pituitary adrenal system and the sympathetic nervous system, respectively. The biological stress response relies heavily on these two systems. In addition, they discovered that yoga reduces anxiety and depressive symptoms in a variety of populations. Yoga also happens to be especially good for them because it can be done in plain clothes, is cheap, and doesn’t take long.
- Having someone to talk to and share difficulties with can also reduce stress. Social support has the potential to reduce stress. Pow et al. (2016) looked at how social support affects paramedics in their work. For a week, 87 participants were required to keep a diary detailing their recognized stress, social support network, and sleep quality. Researchers wanted to see if social support could improve the quality of sleep in their sample because workplace stress can affect sleep quality. It was discovered that over the course of a week, paramedics who reported higher levels of social support also reported better quality sleep, whereas those who reported lower levels of social support reported poor quality sleep.
- Recent research has demonstrated that perceived support from online social networks may also play a role in stress reduction. While it seems obvious that interpersonal social support is important in reducing the effects of stress, A survey of 401 undergraduate students by Nabi, Prestin, and So (2013) found that having more Facebook friends increased perceptions of social support. Then, this was linked to less stress, less physical illness, and better health. This may have something to do with the idea that how people perceive social support is important. A person’s number of Facebook friends should be sufficient as a measure of social support if this is the case. It does not appear that this approach takes into account the quantity or closeness of friendships.
- Social support is culturally dependent as a coping strategy. According to research conducted in 2008 by Kim, Sherman, and Taylor, individuals from various cultures were found to be more or less likely to utilize social support as a coping strategy. 603 adults were studied by researchers. They observed that Asians and Asian Americans were more hesitant to look for help from companions than European Americans since Asian Americans were worried about conceivable adverse results of their solicitation. Therefore, it would appear that cultural differences in how people seek assistance would influence the likelihood of utilizing social support as a stress-relieving strategy.
In a situation, stress can come from a variety of sources, so learning how to manage it effectively—whether through yoga, mindfulness, physical activity, or social support—is crucial. Using these kinds of coping mechanisms on a regular basis can be a good way to protect against the risk factors that come with chronic stress.